How can you identify coronary artery disease (heart artery blockage)
Heart artery blockage is one of the most common heart diseases in our country. It leads to chest pain on exertion, shortness of breath on minimum physical effort, and, if left untreated, often causes heart attacks causing significant heart muscle damage and loss of life. It is essential to detect heart artery blockages at an early stage and treat it adequately to prevent complications and maintain a good quality of care.
The main symptoms of heart artery disease are chest pain or heaviness in the middle of the chest with radiation towards the left arm and jaw. Sometimes the pain can radiate in between the shoulder blade as well. Some people also complain of shortness of breath on exertion. Individuals who smoke , suffer from Diabetes, high blood pressure, or high cholesterol level are more at risk of developing heart artery blockages.
How to diagnose heart artery blockages?
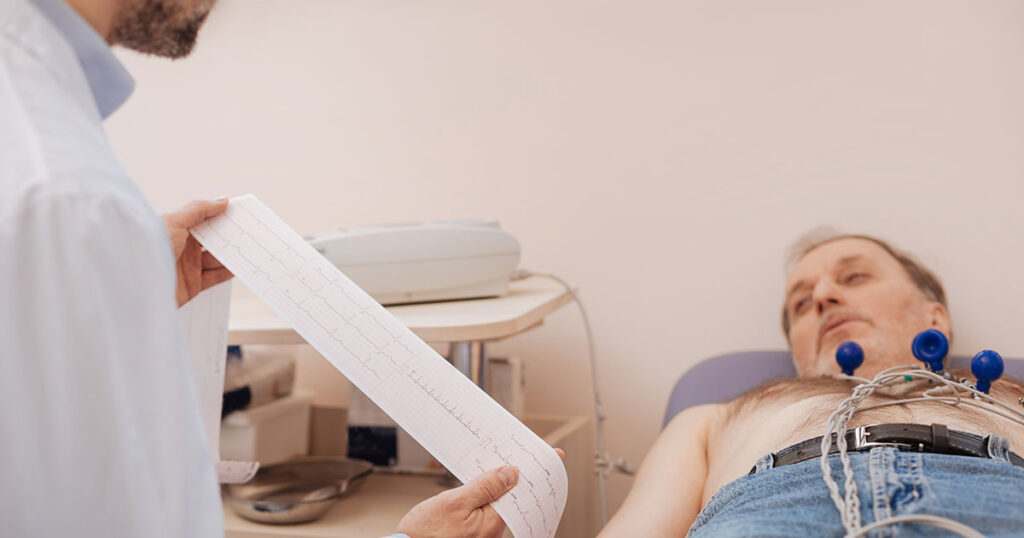
If someone suffers from the symptoms mentioned above, then he/she should consult a doctor. Apart from clinical examination, doctors perform specific tests. ECG is the most commonly used primary test, which doctors often advise. Though a normal ECG does not rule out heart artery blockage, any ECG abnormality helps the doctors to diagnose heart artery blockages. If ECG is normal then doctors often prescribe a TMT (Treadmill test) or a CT coronary angiography as may be necessary. Sometimes your doctor can refer you to an invasive cardiologist (Interventional Cardiologist) to undergo an invasive coronary angiography to diagnose heart artery blockage. Invasive diagnostic coronary angiography is the gold standard test to diagnose heart artery blockage. This procedure is performed by putting a small tube through the wrist artery into the heart after giving some local anesthetic injection to numb the area near the wrist. The small tube (catheter) is engaged inside the heart artery a dye is injected into the artery to visualize the heart arteries and to see the presence of any blockages. Once blockages are detected, the majority of the patients are managed with medicines. Medicines help to improve symptoms of chest discomfort and also prevent further progression of blockages in the future. Along with medications, regular exercise and healthy lifestyle maintenance are very important to remain healthy.
Who requires angioplasty and stenting?
All the patients with heart artery blockages do not require coronary angioplasty and stenting to open up the blockages. Initially, patients can be managed well with medicines. Symptoms can be well controlled only with medication and lifestyle changes. In some of the patients, despite taking medicines, if signs of chest discomfort on exertion, shortness of breath upon any physical activity, or chest heaviness persist, then those patients should be treated with interventional procedures in the form of coronary angioplasty and stenting. Coronary angioplasty and stenting procedure (coronary intervention procedure) can benefit patients with heart attacks or who are suffering from ongoing chest pain at rest (unstable angina). During heart attack coronary angioplasty and stenting gives the best result and ideally this should be performed as soon as possible (primary angioplasty). In this procedure a tube is passed through the wrist or groin artery into the heart artery. The narrowing inside the heart artery is crossed by passing a thin wire through the blockage. A balloon is passed over the wire and inflated at the site of the blockage to open it. A metallic stent (scaffold) is placed at the site of the blockage to keep the artery open. By and large, this procedure is very safe, with an insignificant complication rate of around 1%. Coronary angioplasty and stenting procedure save a life during a heart attack and gives better long term result. Coronary angioplasty improves symptoms in patients with exertional chest discomfort (stable angina) where only medicines are not sufficient. Coronary angioplasty procedure provides a better quality of life and improves exercise tolerance.
Over the last few decades, with the advancement in coronary angioplasty techniques and the invention of a new generation of stents, intervention treatment has become much more accessible and secure. Nowadays, in many occasions, coronary angioplasty and stenting are giving similar benefit where bypass operation used to be the only option. Compared to bypass operation, angioplasty is a much less invasive procedure and does not require to open the chest. This procedure can be performed through a small hole at the wrist artery. Patients get discharged within a day or two. Recovery is speedy, and patients can go back to their healthy life soon.

Is bypass surgery better than angioplasty?
Many times patients ask whether bypass operation is better than angioplasty treatment? The answer to this question cannot be given in a single sentence. The result of treatment varies on different patient characteristics. Traditionally patients with significant blockages in all the 3 arteries or the left main artery (LMS) were better treated with coronary artery bypass surgery for better long term results. Patients with diabetes and blockages in all three arteries are better treated with bypass surgery. Nowadays, many patients are getting an equally good result with multiple stents with blockages in all the 3 arteries and blockages in the main artery (Left main stem). This is possible because of the advent of new stent technologies and equipment in the field of interventional cardiology. An interventional cardiologist can decide on preferred treatment for a patient depending on patient condition and various angiographic parameters.
Nowadays, with the advent of newer technologies, coronary angioplasty can be performed in patients with severe heart artery disease who would have required a bypass operation in the earlier days. New technologies e.g., intravascular ultrasound (IVUS), Optical Coherence Tomography (OCT), are helping us to perform coronary angioplasty and stenting with utmost precision.
How can coronary angioplasty and stent help a patient?
During an acute heart attack, immediate coronary angioplasty and stenting help to save a patient’s life by reestablishing blood flow in the blocked artery. This relieves pain, reduces heart muscle damage, helps the patient to get back to his usual self quickly, and improves long term heart function. This is the best treatment for heart attack today. This procedure must be performed as soon as possible. Delay in treatment can cause permanent damage to the heart. In those places where angioplasty facilities are not available, treatment with clot bursting injection (thrombolysis) is the best alternative treatment. Once clot bursting treatment is initiated, the patient can gain another 24 hours to get himself transferred to a center to have angiography and angioplasty treatment.
In patients with stable angina (patients who suffer from chest pain on exertion), angioplasty and stenting help to improve symptoms in those patients who continue to get chest discomfort and/or shortness of breath despite treatment with medicines. Coronary angioplasty and stenting improve exercise tolerance and quality of life in these types of patients.
Do symptoms of heart disease differ in patients with diabetes?
Diabetes patients are more vulnerable to developing blockages in heart arteries, but they are often not aware of the typical symptom of chest pain of heart artery blockage. Symptoms are often atypical and difficult to diagnose. As a result of lack of symptoms, they may get detected at an advanced stage of the disease. Patients may develop multiple blockages involving all the 3 arteries of the heart. The heart also becomes weak, and pumping ability reduces. If diabetes patients develop atypical chest discomfort and ECG shows any abnormality, then they need to be investigated to rule out any heart artery blockage. A coronary angiography often is required to diagnose the condition. Heart pumping ability usually improves after unblocking the blockages with angioplasty and stenting procedures.
How long patients need to continue medicines?
If patients develop heart artery blockages, they need to continue medicines for an indefinite period. Even after coronary angioplasty and stenting, patients cannot stop the medication. To maintain the patency of the stent, doctors prescribe two antiplatelet (blood-thinning) medicines (Aspirin and Clopidogrel/Ticagrilor/ Prasugrel) for one year. After one year, the Aspirin continues for the indefinite period Clopidogrel/Ticagrilor/Prasugrel can be stopped after consultation with the doctor. Cholesterol-lowering medicines in high dose is another medicine which is necessary to continue for a long time. Patients may require to take a few more medications if the treating doctor feels so.
Is there any risk of performing coronary angiography or angioplasty?
Nowadays, coronary angiography and angioplasty procedures are safe. In the unlikely event, the risks associated with these procedures are heart attack, stroke, bleeding, injury to the arteries, allergic reactions with the dye, kidney failure, and rarely death. In angiography procedure, the severe risks are in a range of 1 in 1000. In coronary angioplasty and stenting procedure, serious risks are in a range of 1%. Majority of the procedures are performed through the wrist arteries hence the chances of bleeding and arterial injuries are often much less. Recovery is also rapid. Patients can be discharged with a day or two of having a stenting procedure. Sometimes patients can be released within 24 hours. Diagnostic angiography procedure through the wrist has enabled the doctors to discharge the patients on the same day.
Coronary angiography and angioplasty procedures have evolved over the last few decades, and it has revolutionized the treatment of heart artery blockages and saved millions of lives. With the advent of newer technologies, these procedures have made the treatment much safer and less painful.